INFORMATION FOR PATIENTS
Naturally regenerate cartilage – with your body’s own cells
Cartilage is essential for the smooth functioning of our joints – so it's a serious problem when this specialized tissue can no longer do its job. Innovative techniques for biological cartilage regeneration can repair cartilage defects naturally.
Our joints are the be-all and end-all when it comes to our mobility. The knee joint in particular works extremely hard every day – and it's one of the most important pillars of our mobility. The Articulating joints such as the knee can only function effectively and without pain thanks to the cartilage between the joint surfaces. If this essential cartilage in the knee or another joint is damaged, it can not only be painful, but also significantly reduce our quality of life.
Innovative products support you with natural cartilage regeneration
Biological cartilage reconstruction procedures, such as matrix-associated autologous chondrocyte implantation (M-ACI), use your own cells to regenerate the damaged cartilage. To achieve this, we develop intelligent biomaterials that are used to produce an individualized cell graft using your autologous cartilage cells that is then transplanted into the defect.
How exactly does it work? On this page we show you how treatment with autologous cartilage cell implantation works step-by-step. Before we explain this treatment in detail, let’s take a small step back: What exactly is cartilage, what does it do and how does it become damaged?
Keeping your joints working: Hyaline cartilage
Healthy cartilage tissue (hyaline cartilage) has exeptional shock absorbing an a frictionless properties that allows smooth, pain-free joint movement. Ist is a highly pressure-resistant an elastic tissue that consists of 80% water and a very small volume of cartilage cells known as chondrocytes.
Chondrocytes from a network of crosslinked collagen fibres alng with specialized carbohydrate decorated proteins (proteoglycans) that attract and bind water forming an elastic tissue that protects the joint against pressure. Viewed under the microscope, cartilage tissue is a three-dimensional structure made up of collagen and proteoglycans interspersed with chondrocyte cells.
How does cartilage damage occur?
You are not alone in having damaged cartilage tissue: around 6 million people are affected worldwide every year and around 30,000 cartilage treatments are performed in Germany alone. That’s why we specilaize in developing innovative products that enable you to experience natural and atraumatic cartilage regeneration.
Cartilage defects are usually caused by twisting of the knee that also damages other joint stabilizing structures (ligaments and meniscus). Underlying bone pathologies such as osteochondritis dissecans (OCD) can also lead to damages to the protective cartilage surface. If left untreated, early stage damage (osteoarthrosis) progresses to a more painful and functionally debilitating inflammatory osteoarthritis condition.
| Warning: The treatment methods described on this page involving biological cartilage regeneration cannot be used in advanced osteoarthritis. |
|---|
Why can the cartilage not regenerate itself?
This is because mature cartilage has no blood supply and very few chondrocytes available to repair the damage. The repair tissue that does form in some cases serves more as a short term scar tissue that does not have the shock absorbing, frictionless properties of healthy hyaline cartilage.
What procedures for treating cartilage damage are available?
Cartilage defect diagnosis and therapy
If you suspect a cartilage defect, your doctor can use imaging techniques, such as MRI, to make a reliable diagnosis and to determine the precise extent of the damage. When it comes to cartilage damage, an ounce of prevention is generally worth a pound of cure: clinical studies have shown that osteoarthritis risk increases dramatically with larger cartilage defects that are not treated promptly or correctly.
Conservative (non-surgical) forms of therapy, such as targeted physiotherapy, pain relief with non-steriodal anti-inflammatory (e.g., ibuprofen, acetominophen), injections of corticosteroids or viscosupplements such as hyaluronic acid, may temporaly relieve pain and restore function. Once these conservative approaches start to fail, surgical treatment is the only option.
Today there are several surgical procedures available – your doctor will discuss with you which of these options is the right one for your individual case.
Microfracture surgery
Microfracture surgery can be considered for small cartilage damage up to 2 cm2 in size. The bone underneath the cartilage defect is perforated using special drills or chisels, allowing blood from the bone marrow to enter the defect area and coagulate there. This stimulates the formation and form a blood clot. Stem cells within the clot form a fibrous repair tissue and does not have the same pressure-resistance and elastic properties as healthy hyaline cartilage.
Matrix-augmented bone marrow stimulation
This procedure describes microfracture surgery in which the defect is additionally covered with a biomaterial, usually a collagen matrix. This helps anchor the blood clot within the defect and reduces the risk of shearing or loosening of the clot. However, as with microfracture surgery without biomaterial, usually only fibrous cartilage is generated.
Autologous osteochondral implantation
This method transfers healthy bone-cartilage plugs from non-weight-bearing regions of your joint to your damaged cartilage area. The method, also known as mosaicplasty, can be used for minor cartilage damage. It is generally no longer recommended for defects larger than 2 cm2, as the use of several punch cylinder biopsies results in an incongruent (non-matching) surface in the treated defect area, which significantly increases the resulting risk of osteoarthrosis.
Autologous chondrocyte implantation – ACI
Modern transplant procedures, such as autologous chondrocyte implantation (ACI), offer the possibility of regenerating cartilage damage using cartilage cells from your own body. A solution of chondrocytes harvested and grown in culture from a small sample of your own cartilage tissue are placed into the cartilage defect and covered with a water-tight membrane to keep them in place. These procedures are minimally invasive, joint-preserving and offer patients many other advantages.
What is the M-ACI procedure?
What are the advantages of autologous chondrocyte implantation?
The implantation of autologous cartilage cells for the treatment of cartilage damage has been tried and tested for over 20 years. We can now achieve success rates of over 90% with our ACI products. Numerous published clinical studies have shown that ACI is significantly superior to the methods described above, especially in the case of larger defects and after longer progression times. That is why it is recommended as the preferred treatment method by various professional associations in suitable indications[1] and defects larger than 2-3 cm2.
The newest version of ACI, known as matrix-associated ACI (M-ACI), uses a carrier delivery system (three-dimensional collagen matrix) to implant your chondrocytes. This significantly simplifies the implantation surgery and also supports the natural regeneration of new and healthy cartilage tissue. Other promising advantages include:
- The ability to also biologically reconstruct larger cartilage defects without the risk of damage to the donor site, as only a very small amount of your own healthy cartilage tissue is needed.
- Numerous published clinical studies demonstrate the long-term durable pain and functional outcomes of this method.
How does matrix-associated ACI work?
The M-ACI procedure essentially consists of three steps: biopsy, production and quality assessment of your personalized cartilage graft, and subsequent implantation into the defect area. Minimally invasive surgery is required for the first and last step.
How M-ACI works
Step 1: Biopsy of cartilage
- The surgeon arthroscopically collects small pieces of healthy cartilage from a non-weight bearing region of the joint.
- The tissue collected is then sent to our production area.
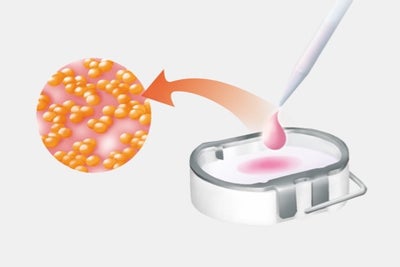
Step 2: Cultivation of the chondrocytes
- The chondrocytes are isolated from the biopsy and propagated in our production facility.
- The cultured chondrocytes are allowed to attach to the collagen matrix. The final biologic product is inspected and tested for quality and then returned to the surgeon for implantation. Strict sterility parameters are maintained and tested throughout the entire process.
- Production of your personalized cell graft is completed approximately 3 weeks after biopsy.
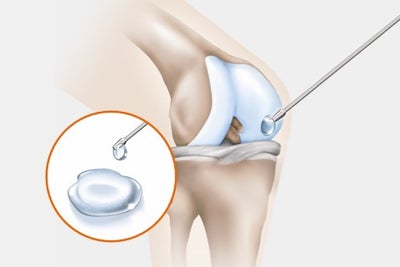
Step 3: Cartilage cell implantation
Inpatient hospitalization with short surgical operation:
- A small incision (mini-arthrotomy) is used to access your joint space, all damaged cartilage is removed form the defect area.
- Customized instrumentation is used to size your cartilage graft to match the defect.
- The graft is placed into the defect and anchored in place with a few sutures.
- The joint is flexed and extended several times to ensure that the graft stays in place.
- The incision is then closed.
Matrix-associated chondrocyte implantation
Our innovative biomaterials specially developed for the MACI procedure provide provide both implantable and injectable options for the delivery of autologous chondrocytes: a collagen matrix or a self-polymerizing hydrogel.
The former uses a three-dimensional collagen matrix. The cultured chondrocytes are allowed to attach to the matrix and the graft is cut to the shape of the cartilage defect.
In the other matrix-associated ACI variant, the cultured chondrocytes are mixed into a hydrogel and then injected into the defect area. After a short time, the hydrogel solidifies and anchors the cells in the defect.
When is M-ACI used?
Chondrocyte implantation is generally suitable for the surgical biological reconstruction of full-thickness cartilage damage in the knee joint. In addition to the size of the defect and the condition of the cartilage, other individual factors play an important role. Which therapy is the right one for a knee cartilage defect is also determined by factors such as biological age, lifestyle and body weight.
Your specialist will determined whether and under what conditions M-ACI is right for you following a thorough examination. The effects of the individual factors must assessed by the orthopaedist treating you.
Are you interested in chondrocyte implantation?
| Please contact your cartilage specialist for further information and details on treatment. Please discuss whether you are eligible for M-ACI therapy with your doctor. |
|---|
Follow-up treatment
What do you need to consider after treatment with the M-ACI procedure?
Postoperative follow-up after cartilage cell implantation depends primarily on the anatomical location of the cartilage defect within the knee joint. The cartilage must first heal completely in this position in order to be able to optimally perform its task as a shock absorber for the joint again. Gradual muscular stabilization of the joint is extremely important and can take a long time.
Since everyone reacts differently to a surgical procedure, the follow-up treatment program can vary from patient to patient. Bed rest in the first few days after the operation, generally avoiding loading the knee joint by using walking aids and accompanying physiotherapy over the next few weeks form the general framework of the follow-up treatment. Your doctor will work out the appropriate measures for you after the operation.
Follow-up assessments
To ensure the long-term success of cartilage regeneration, follow-up checks are recommended at regular intervals. In addition to the clinical follow-up assessment, an MRI examination 3 and 12 months after implantation is recommended in line with recommendations of medical associations.
| Glossary | Explanation | Abbreviation |
| ACI | Autologous chondrocyte implantation, also known as autologous chondrocyte implantation or autologous cartilage cell implantation. This procedure is used to treat cartilage damage. Autologous cartilage cells are collected, cultured in a nutrient solution and inserted into the patient’s cartilage defect in order to reduce the discomfort caused by the cartilage damage and prevent the development of osteoarthrosis. | ACI |
| Matrix-associated ACI | Also commonly referred to as: matrix-coupled, matrix-supported or matrix-induced autologous chondrocyte implantation (MACI). In the MACI procedure, the cultivated autologous cartilage cells are implanted into the defective cartilage area using a carrier medium, such as a collagen matrix or a hydrogel. | MACI M-ACI ACI-M |
| Autologous | From the same body | |
| Chondrocytes | Cartilage cells or tissue from the same individual | |
| In-situ | Retention (of implanted cells) in the desired position in the body |
[1] Niemeyer P, Albrecht D, Andereya S, Angele P, et al. Autologous chondrocyte implantation (ACI) for cartilage defects of the knee: A guideline by the working group "Clinical Tissue Regeneration" of the German Society of Orthopaedics and Trauma (DGOU), The Knee, Review 23,426-435(2016) https://doi.org/10.1016/j.knee.2016.02.001